Understanding Obesity Surgery: A Critical First Step
The first step in preparing for obesity surgery is to thoroughly understand what the procedure entails. Obesity surgery is a significant medical intervention aimed at helping individuals with severe obesity achieve sustainable weight loss and improve associated health conditions. These surgeries work by altering the digestive system, reducing the stomach’s capacity or modifying nutrient absorption. Common types of obesity surgery include gastric bypass, sleeve gastrectomy, and gastric banding. Each method comes with specific advantages, risks, and recovery processes. It’s crucial to learn about these options and discuss them with your healthcare provider to ensure you select the procedure that best suits your needs and lifestyle. This understanding sets the foundation for the journey ahead, allowing you to have realistic expectations and a clear sense of purpose as you move forward.
Consulting with Healthcare Professionals
Before undergoing obesity surgery, consulting with a team of healthcare professionals is essential. This often includes a surgeon, dietitian, psychologist, and sometimes a physician specializing in obesity. During these consultations, you will receive a complete medical evaluation to assess your readiness for obesity surgery based on your health history, current medications, and existing medical conditions. It’s also an opportunity to address any questions or concerns you may have about the surgery and recovery process. Understanding the risks and benefits of obesity surgery from your healthcare team’s perspective will give you the confidence and knowledge necessary to move forward with the procedure. These professionals will also help you set realistic goals and expectations for your post-surgery lifestyle.
Setting Realistic Goals for Weight Loss
Setting achievable and realistic goals is a key component in preparing for obesity surgery. Weight loss after surgery varies from person to person, but most patients lose 50% to 70% of their excess weight in the first year. These results depend on several factors, including the type of obesity surgery, adherence to post-surgery guidelines, and individual metabolism. While it is important to be excited about the transformation, patients should understand that rapid weight loss can also present challenges such as skin sagging or emotional adjustments. Establishing long-term goals—such as adopting healthier eating habits, staying active, and attending regular follow-up appointments—will help ensure that your obesity surgery leads to lasting success. Embrace the journey as a gradual process, not just a destination.
Preparing Mentally for the Changes Ahead
Mental preparation is just as important as physical readiness when preparing for obesity surgery. Many patients experience a range of emotions before and after surgery, including excitement, fear, and anxiety. Understanding the psychological impacts of obesity surgery can help you manage these emotions. You may also experience changes in body image as the weight comes off quickly, and it is essential to be prepared for the psychological aspects of this transformation. Support groups, therapy, and counseling are valuable resources to help you navigate these changes and address any emotional eating habits. Preparing yourself emotionally ensures that you have the resilience to follow through with the necessary lifestyle changes and to fully embrace the physical and mental improvements that will come with your new life.
Nutrition and Diet Preparation
Proper nutrition and diet preparation are integral to the success of obesity surgery. In the weeks leading up to your surgery, you will be given specific dietary instructions, which typically include reducing caloric intake and eliminating certain foods. Following a pre-surgery diet can help prepare your body for the surgery and reduce the risk of complications during the procedure. After the surgery, your diet will be gradually transitioned from liquids to pureed foods and eventually to solid foods. Adopting these new eating habits is crucial for the long-term success of obesity surgery. You will be required to avoid high-calorie, high-sugar foods, and focus on a balanced diet that includes lean proteins, vegetables, and healthy fats. Partnering with a dietitian can help you develop a post-surgery nutrition plan that meets your specific needs.
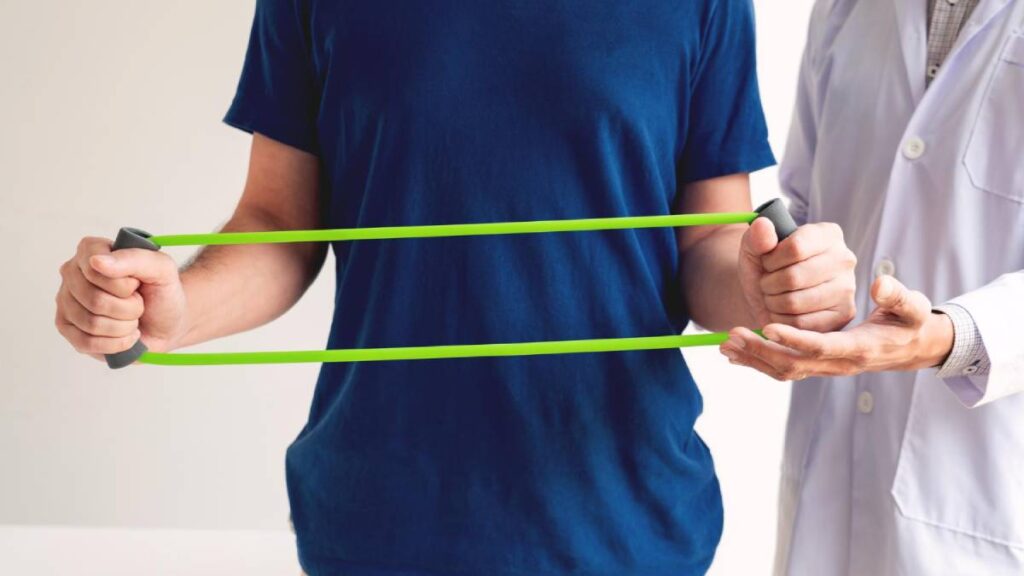
Physical Activity and Exercise Preparation
Physical activity is a cornerstone of successful long-term weight management following obesity surgery. Leading up to your surgery, incorporating light exercises into your routine can help improve overall fitness and prepare your body for recovery. After surgery, you will be encouraged to start with gentle movements like walking to prevent blood clots and improve circulation. Gradually, you will be able to increase the intensity and duration of your exercise routine. Regular physical activity, including strength training and cardiovascular exercises, will help you maintain muscle mass, improve cardiovascular health, and boost overall well-being. Staying active not only supports weight loss but also contributes to mental clarity and emotional stability, making exercise an essential part of the post-surgery lifestyle.
Post-Surgery Support and Follow-Up Care
Once your obesity surgery is complete, ongoing support and follow-up care are critical to ensuring success. This includes regular visits to your healthcare team, including your surgeon, dietitian, and mental health professional. Follow-up appointments help monitor your progress, manage any complications, and provide necessary adjustments to your post-surgery care plan. Many patients benefit from joining a support group or connecting with others who have undergone similar surgeries. These groups can provide emotional support and practical advice, helping you stay motivated and on track with your goals. Post-surgery support ensures that you continue making the necessary changes to maintain a healthy weight and lifestyle, ultimately leading to a successful long-term outcome.
Conclusion
Preparing for obesity surgery is a multi-faceted process that requires careful planning, education, and mental preparation. By understanding the surgery, setting realistic goals, adjusting your diet, and committing to physical activity, you are setting yourself up for a successful journey. Keep in mind that obesity surgery is not a quick fix, but rather a tool that will help you achieve long-term weight loss and better health. With proper support and adherence to new lifestyle changes, you can experience significant improvements in both your physical and mental health. The road ahead requires dedication, but the rewards—improved quality of life, reduced health risks, and greater self-esteem—are well worth the effort. Approach your obesity surgery journey with a positive and determined mindset, and you will be well on your way to a healthier future.
Frequently Asked Questions
- How long is the recovery time after obesity surgery?
- Recovery time varies, but most patients return to light activities within 2–4 weeks and full recovery within 6–8 weeks.
- Do I have to follow a strict diet after surgery?
- Yes, post-surgery, you’ll follow a strict diet that gradually transitions from liquids to soft solids to ensure safe healing.
- Is it necessary to exercise after obesity surgery?
- Yes, regular exercise is essential for long-term weight maintenance and overall health improvement.
- How much weight can I expect to lose after surgery?
- Most patients lose 50% to 70% of their excess weight within the first year following surgery.
- Can I regain weight after obesity surgery?
- Weight regain is possible if unhealthy eating habits are resumed, but maintaining a healthy lifestyle helps prevent it.
- Will I need to take vitamins after obesity surgery?
- Yes, lifelong vitamin and mineral supplementation is typically required to avoid nutritional deficiencies.
- Is obesity surgery covered by insurance?
- Many insurance plans cover obesity surgery if it is deemed medically necessary and the patient meets specific criteria.
- How do I know if I’m a candidate for obesity surgery?
- Candidates generally have a BMI of 40+ or 35+ with obesity-related health issues, and have unsuccessfully tried other weight loss methods.
- What is the best type of obesity surgery for me?
- The best option depends on your health, weight loss goals, and the recommendations of your surgeon.
- Will I need emotional support after obesity surgery?
- Yes, emotional support through therapy or support groups can be helpful for adjusting to the changes and maintaining success.